
Thinking, fast or slow? Reasoning strategies in medical diagnosis
This blogpost was written by Berry Van Den Berg and Jos Snoek
Doctors often have to make diagnoses based on fuzzy or incomplete information, under time pressure or other difficult circumstances, and a correct diagnosis is the important starting point for effective therapy. Although the way doctors diagnose their patients has been a subject of research for decades, many unanswered questions remain and many theoretical models have been proposed and used. To investigate the neural mechanisms underlying decision making, we conducted a study in which experienced neurologists where solving cases while we simultaneously measured their brain activity (van den Berg, de Bruin, Marsman, Lorist, Schmidt, Aleman & Snoek, 2020).
In this study, we sought to investigate differences on a neural level between two hypothesized modes of reasoning, one fast and effortless, the other slow and deliberate. This model of reasoning (dual process) has become widely popular (see Kahneman’s bestselling book Thinking, fast and slow 2011). A good reason to acquire some empirical data and shed light on the neural underpinnings of the dominant dual process theory, a theory which has formed the basis of dozens of studies in medical education and educational and social psychology.
Doctors have been found to rely heavily on fast pattern-recognition based reasoning (referred to as Type 1 reasoning), using so-called ‘illness-scripts’, when confronted with a medical problem. Only when they do not recognize the problem to be solved as a common, more or less typical case, they revert to the more effortful and slow strategy of analytical reasoning (Type 2). Imagine the case of a 28-year old woman with numbness below the waist present from the minute she wakes up. She needs support when walking. She has had an episode of transient vision loss in one eye, two years ago. She also has had a period of facial pain a year ago. She has not urinated since getting up. On examination she has normal strength in her legs. On sensory testing, she has diminished sense of touch from halfway her abdomen. Reflexes in her legs are exaggerated and the plantar reflex is abnormal. Her spinal fluid shows a normal cell count and an increased IgG-index. This is a typical pattern for a diagnosis of multiple sclerosis. What would happen if we replace the fourth item (transient loss of vision) for other information? What if instead she has been treated for a tick bite (suggesting Lyme disease) a year prior to her visit? In this case, the diagnosing neurologist not only loses one typical MS feature, but also has to deal with a new, conflicting item. One may expect that such diagnostic ‘noise’ results in a shift from Type 1 reasoning to Type 2 reasoning; to a longer diagnostic process and to less certainty about the correct diagnosis of multiple sclerosis. This is exactly what we found, behaviorally, both in a validation-pilot study and in our recent fMRI-study. The hypothetical case described above is one of the cases we presented to sixteen experienced neurologists, who solved them inside an MRI scanner.
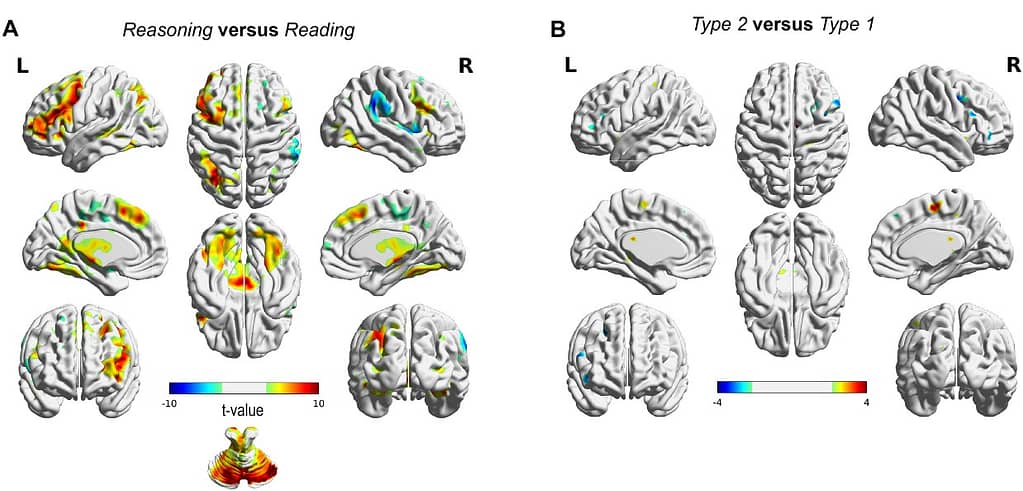
Blood oxygen level-dependent imaging activity differences. (A) Reasoning (Type 1 cases and Type 2 cases together) showed activity in caudate nucleus, left prefrontal, parietal and cerebellar regions. (B) Activity difference map between Type 1 and Type 2 cases. No significant difference was found at P < 0.05 (FWE corrected).
When we analyzed their fMRI data, we did not find pronounced differences in terms of regional activation between the typical and atypical cases (which is what you would expect if different processes were used). However, notable differences were observed in functional connectivity. Among those: cases containing ambiguous information showed stronger connectivity between specific regions in the frontal, parietal, and temporal cortex in addition to the cerebellum. These regions have been associated to be key nodes in networks sub-serving executive control functions such as attention and working memory.
These results were puzzling: on one hand we did not find what we expected, that is differences in activation between the different types of cases (as one would expect for different types of reasoning). We did find differences in the way individual brain areas communicated. So how can we interpret these findings?
Well, one prominent theory in neuroscience suggests that the brain continuously predicts and anticipates future events and information. This theory fits quite nicely with the idea of schematic anticipation by Otto Selz (Selz, 1922), developed in the early years of the 20th century. In short: when confronted with a diagnostic problem, the physician(’s brain) anticipates the solution, the correct diagnosis, by creating a schema, a mental representation of the most likely illness. Clinical experience plays a pivotal role in this largely automatic process and determines the quality of this early case building. In the case that information is overall consistent with this early, provisional diagnosis, the gap between early and final diagnosis is absent or minimal. However, when information is not representative of this schema the brain relies on executive networks to figure out how to interpret this information, and if necessary, to seek for additional information (for instance, from memory), and to update (or not to) the anticipated schema(s). Schematic anticipation has been a particular useful concept in research here in Groningen on (chess) expertise (de Groot, 1946, 1965, 1986). Recent theories in neuroscience suggest that neural predictive encoding may share key conceptual elements with this theory of schematic anticipation. As such, an almost forgotten century-old, but –in our opinion– attractive theory on human reasoning may be strengthened and revitalized by experimental neuroscience.
We hope that these results, together with future studies, will provide empirical evidence that guides and unifies theories on medical reasoning and more general reasoning processes. Ultimately, we think that studies with an interdisciplinary perspective like this one can guide how we think about medical reasoning, and thus may provide the background for the design of medical educational programs. Conceptually, making a distinction between fast and slow might be appealing because of its simplicity. On a neural level, this distinction does not work so well, and a more dynamic anticipatory view fits better with the data, ties into old ideas regarding reasoning, and fits well with current theories of brain functioning.
References
de Groot, A. D. (1946). Het denken van den schaker: een experimenteel-psychologische studie (p. 315). Amsterdam: Noord-Hollandsche Uitgevers Maatschappij.
de Groot, A. (1965). Thought and Choice in Chess (2nd ed.). The Hague: Mouton Publishers.
de Groot, A. D. (1986). Intuition in chess. ICGA Journal, 9(2), 67-75.
van den Berg, B., de Bruin, A., Marsman, J-B. C., Lorist, M., Schmidt, H., Aleman, A., & Snoek, J. (2020). Thinking fast or slow? Functional magnetic resonance imaging reveals stronger connectivity when experienced neurologists diagnose ambiguous cases. Brain Communications, 2(1).
Selz, O. (1922). Zur Psychologie der produktiven Denkens und des Irrtums. Cohen, Bonn.



