Update: Metacognition in Psychotic Disorders: Grounds for Therapy?
Since the introduction of antipsychotic medication in the 50’s, add-on psychotherapy for persons with a psychotic disorder has slowly become part of the treatment guidelines, and the prognosis for psychotic disorders has improved dramatically. Nonetheless, there is much left to be gained: Many persons do not seem to benefit from the range of interventions available. For instance, negative symptoms (I will discuss these below) are notoriously difficult to treat, as are patients who suffer from extreme disorganization. One promising avenue of research has taken the attention in psychotherapy away from reducing symptomatology (for instance, hearing voices) or training skills (such as social skills) and seeks to take a more process-oriented approach.
“The prognosis for psychotic disorders has improved dramatically. Nonetheless, there is much left to be gained.”
Before discussing these types of therapy, let’s first turn to the topic of psychosis. According to the Diagnostic and Statistical Manual for Mental Disorders – 5 (DSM-5), persons with a psychotic disorder typically experience symptoms which distort reality. Positive symptoms add to the behavioral repertoire and include hearing voices. Negative symptoms subtract from behaviors and include the inability to experience pleasure from something that was previously considered enjoyable. It is important to note that classification systems such as the DSM-5 generally produce a clearer picture of psychological difficulties (psychopathology) than can be found in reality (see Selwyn Renard’s recent blog post for an example). Persons with a disorder in the psychosis spectrum usually also suffer from symptoms that constitute more general psychopathology, such as depression.
For instance, in addition to negative and positive symptoms, it has been found that persons with a psychotic disorder frequently exhibit difficulties with ‘metacognitive capacity’ – thinking about thinking and feeling in oneself and others. Forming an accurate picture of what is going on within yourself is not an easy feat for anyone!
“In recent years, scientists and clinicians have developed several types of psychotherapy … One such therapy is Metacognitive Reflection and Insight Therapy (MERIT).”
Metacognition has been conceptualized to include four domains (Semerari et al., 2003): The first is being able to think about your own thoughts and feelings, and incorporating those into an idea about who you are and how you are doing (Self-Reflectivity). The second domain is the ability to do the same, but about other people (Understanding the Other’s Mind). The third metacognitive capacity is the ability to understand that other people have radically different lives, which have nothing to do with you and being able to place yourself in this much larger world (Decentration). The fourth brings all this information together, in the ability to detect when you have psychological distress, and finding adequate ways of coping with these stresses (Mastery).
In recent years, scientists and clinicians have developed several types of psychotherapy based on this or similar models (Hamm, Hasson-Ohayon, Kukla, & Lysaker, 2013). One such therapy is Metacognitive Reflection and Insight Therapy (MERIT). Put very briefly, the therapist asks a client to share what is on their mind. This usually leads to a conversation about events that previously occurred in the client’s life. By monitoring the level of metacognitive functioning of the client, the therapist is able to ask questions at this level or slightly above it. For instance, a client is able to differentiate between her own cognitive operations, but is unable to form a nuanced idea about her emotions. Such a client would be able to say “I remember I thought people were all looking at me”, but would have difficulty explaining which emotion this caused. For instance, she may have felt fear because they may all think they want to rob her, may have felt anger because she just wants to be left alone, or felt worthless because she feels they are all much more successful than she is. The therapist would ask questions like: “So when you walked in, you thought ‘boy, there sure are a lot of people here’ and ‘I really wish I wasn’t here’. In a previous session you mentioned that you think people generally want to hurt you. Were you afraid of the people?” (Lysaker et al., 2014).
“Our most important findings have been that MERIT seems to work even with clients who present with relatively chronic problems or many negative symptoms, who typically do not respond well to treatment.”
Several research teams around the world have started experimenting with the method. Our research team has been conducting one such trial (Van Donkersgoed et al., 2014). First, we determined that we could train therapists and that those therapists would also have good results with the method. (de Jong et al., 2015). We published two case studies, one describing the outcomes with a severely disorganized patient and one with a patient suffering from severe negative symptoms (de Jong et al., 2016; van Donkersgoed, de Jong, & Pijnenborg, 2016). Our most important findings have been that MERIT seems to work even with clients who present with relatively chronic problems or many negative symptoms, who typically do not respond well to treatment.
The second step has been to train 13 therapists in 7 different mental healthcare facilities in the Netherlands and include 70 persons with schizophrenia or schizoaffective disorder to participate in the study. Of these 70 participants, 35 were offered MERIT, while the other 35 functioned as a control group, and had to wait to start their treatment, so we could compare what difference the treatment makes to the usual care. We are now nearing the end of the trial, collecting the last data, and hope to be able to report our findings soon, including on this blog. Keep your eyes peeled for another update!
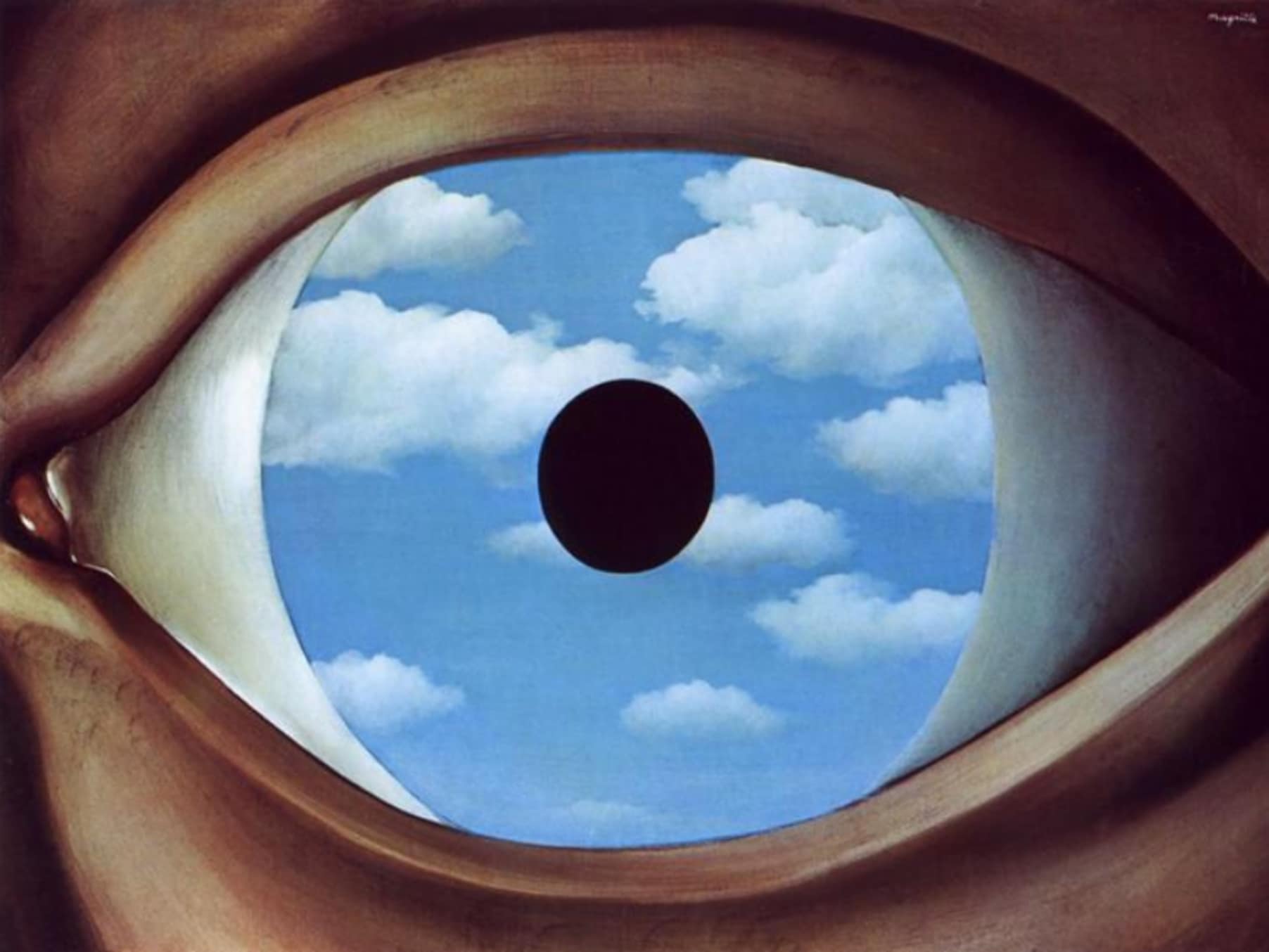
Note: Image with permission from Ashley de Jong-Doucette: http://dejongdoucette.com.
References:
Bargenquast, R., & Schweitzer, R. D. (2013). Enhancing sense of recovery and self-reflectivity in people with schizophrenia: A pilot study of Metacognitive Narrative Psychotherapy. Psychology and Psychotherapy, doi:10.1111/papt.12019
Corcoran, R., Mercer, G., & Frith, C. D. (1995). Schizophrenia, symptomatology and social inference: investigating “theory of mind” in people with schizophrenia. Schizophrenia Research, 17(1), 5–13.
de Jong, S., Donkersgoed, R. J. M. van, Aleman, A., van der Gaag, M., Wunderink, L., Arends, J., … Pijnenborg, G. H. . (2015). The practical implications of Metacognitive psychotherapy in psychosis: findings from a pilot study. Journal of Nervous and Mental Disease, accepted.
de Jong, S., van Donkersgoed, R., Pijnenborg, G. H. M. H. M., Lysaker, P. H., Jong, S., Donkersgoed, R., … Lysaker, P. H. (2016). Metacognitive Reflection and Insight Therapy (MERIT) with a patient with severe symptoms of disorganization. Journal of Clinical Psychology, doi:10.1002/jclp.22249
Hamm, J. A., Hasson-Ohayon, I., Kukla, M., & Lysaker, P. H. (2013). Individual psychotherapy for schizophrenia: trends and developments in the wake of the recovery movement. Psychology Research and Behavior Management, 6, 45–54. doi:10.2147/PRBM.S47891
Lysaker, P. H., Buck, K. D., Leonhardt, B. L., Buck, B., Hamm, J., Hasson-Ohayon, I., … Dimaggio, G. (2014). Metacognitively focused psychotherapy for people with schizophrenia: Eight core elements that define practice. In P. H. Lysaker, G. Dimaggio, M. Brüne, P. H. (Eds.), Social cognition and metacognition in schizophrenia: Psychopathology and treatment approaches. (pp. 195–213). San Diego, CA, US: Elsevier Academic Press.
Lysaker, P. H., Buck, K. D., & Ringer, J. (2007). The recovery of metacognitive capacity in schizophrenia across 32 months of individual psychotherapy: A case study. Psychotherapy Research, 17(6), 713–720. doi:10.1080/10503300701255932
Penn, D. L., Sanna, L. J., & Roberts, D. L. (2008). Social cognition in schizophrenia: an overview. Schizophrenia Bulletin, 34(3), 408–11. doi:10.1093/schbul/sbn014
Van Donkersgoed, R. J., De Jong, S., Van der Gaag, M., Aleman, A., Lysaker, P. H., Wunderink, L., & Pijnenborg, G. (2014). A manual-based individual therapy to improve metacognition in schizophrenia: protocol of a multi-center RCT. BMC Psychiatry, 14(1), 27. doi:10.1186/1471-244X-14-27
van Donkersgoed, R. J. M., de Jong, S., & Pijnenborg, G. H. M. (2016). Metacognitive Reflection and Insight Therapy (MERIT) with a patient with persistent negative symptoms. Journal of Contemporary Psychotherapy, 72(2), 164–174. doi:10.1007/s10879-016-9333-8
van Veluw, S. J., & Chance, S. A. (2014). Differentiating between self and others: an ALE meta-analysis of fMRI studies of self-recognition and theory of mind. Brain Imaging and Behavior, 8(1), 24–38. doi:10.1007/s11682-013-9266-8