Treatment of complicated grief:
Moving a research field forward
The death of a loved one can be an emotionally overwhelming life-event, one that most people experience during their lifetime. While many people adjust to their loss after acute grief subsides, a minority experiences severe, enduring, and disabling grief symptoms. Only since the mid-nineties, clinicians and researchers have attempted to define these loss reactions, often termed complicated grief. Evidence is accumulating that complicated grief is conceptually distinct from related mental health problems such as depression and post-traumatic stress disorder and requires specific treatment.
“complicated grief is conceptually distinct from related mental health problems such as depression and post-traumatic stress disorder”
In 2013, Persistent Complex Bereavement Disorder (PCBD) was included into the DSM-5 as a diagnosis for further investigation. A similar diagnosis, Prolonged Grief Disorder (PGD), will probably be included in the 11th International Classification of Diseases (ICD-11), scheduled to be released in 2018. Core symptoms of PGD include persistent and pervasive yearning for a lost loved one and a strong preoccupation with this person beyond 6 months after bereavement. PGD is further characterized by anger about the death, feelings of guilt, difficulties accepting the loss, and difficulty in engaging in new activities.
Proponents of inclusion of a complicated grief disorder in diagnostic manuals argue that it will stimulate research of grief-specific treatments, and – perhaps more importantly – integration of such treatments into mental health care. However, researchers, health care professionals, and members of the general public alike have mentioned potential drawbacks such as risks of overdiagnosis and misdiagnosis, and stigmatization.
“we found no evidence for the idea that all bereaved people, irrespective of symptom levels, would benefit from intervention”
In a recent review of complicated grief treatments (Doering & Eisma, 2016), we found no evidence for the idea that all bereaved people, irrespective of symptom levels, would benefit from intervention. Further, evidence was mixed for the treatment of bereaved people at risk of complicated grief (e.g., because their loved one died by suicide). Moreover, while depression and anxiety medications are often prescribed to bereaved people, there is no conclusive evidence that this reduces complicated grief. Nevertheless, interventions that specifically focus on people who report severe distress (e.g., meet criteria for PGD) are effective, and the most promising treatment is cognitive-behavioral therapy (CBT).
CBT is based on a model which assumes the persistence of complicated grief is due to interacting changes in three core processes: negative cognitions, avoidance behaviors, and autobiographical memories. For example, a person may irrationally believe that experiencing negative emotions related to the loss may lead oneself to ‘go crazy’ or ‘lose control’. Consequently, such negative misinterpretations of emotions could contribute to the suppression of memories that remind of the deceased (e.g., memories about events related to the death). This, in turn, may lead to insufficient cognitive elaboration of the loss, which prolongs distress and impairs one’s ability to integrate loss-related memories with existing autobiographical knowledge to create a meaningful life-story. In line with this model, CBT treatment of complicated grief typically consist several components, including challenging of negative beliefs and misinterpretations; (gradually) confronting persons with avoided aspects of the loss (e.g., through exposure exercises); and creating an autobiographical loss story.
“while research generally supports the effectiveness of CBT, it usually only yields clinically-relevant changes in complicated grief symptom levels in up to about half of people with complicated grief”
Importantly, while research generally supports the effectiveness of CBT, it usually only yields clinically-relevant changes in complicated grief symptom levels in up to about half of people with complicated grief. This suggests that the treatment of complicated grief can be improved. Unfortunately, insight into how to enhance treatment is hampered because of limited knowledge about what interventions work best for whom, and how they work.
To understand what works best, we recommended conducting large-scale, stepped treatment effectiveness studies in which the effects of (components of) successful treatments for complicated grief are compared. For instance, previous studies have shown that exposure is particularly effective, as it yielded additional effects over and above CBT without exposure. Interestingly, stand-alone brief online exposure also strongly reduces complicated grief.
“specific information about subgroups for which CBT for complicated grief works best is still lacking”
Additionally, we can find out who benefits most from which intervention by analyzing if there are specific subgroups for which certain interventions work better. While meta-analyses thus far appear to indicate that apart from distress levels few variables influence the effect of grief interventions, specific information about subgroups for which CBT for complicated grief works best is still lacking. Filling this gap in knowledge would enable development of personally-tailored treatments.
Lastly, by experimentally testing the theories of how treatments work, and by conducting mediator analyses of treatment effectiveness studies, we can examine which working mechanisms underlie the effects of CBT for complicated grief, and thereby which processes we should target in therapy. Preliminary studies indicate that reductions in negative cognitions and avoidance behavior are associated with CBT treatment effects, but more research is warranted.
Taken together, these research lines could create a broad evidence base for treatments that could inform optimal treatment of distressed bereaved persons. The importance of this should not be understated, as the inclusion of PGD in the ICD-11 will likely lead to a strong demand for protocolled, easily administrable, evidence-based treatments by clinicians and policy makers.
References
Doering, B. K., & Eisma, M. C. (2016). Treatment for complicated grief: State of the science
and ways forward. Current Opinion in Psychiatry, 29(5), 286-291.
Note
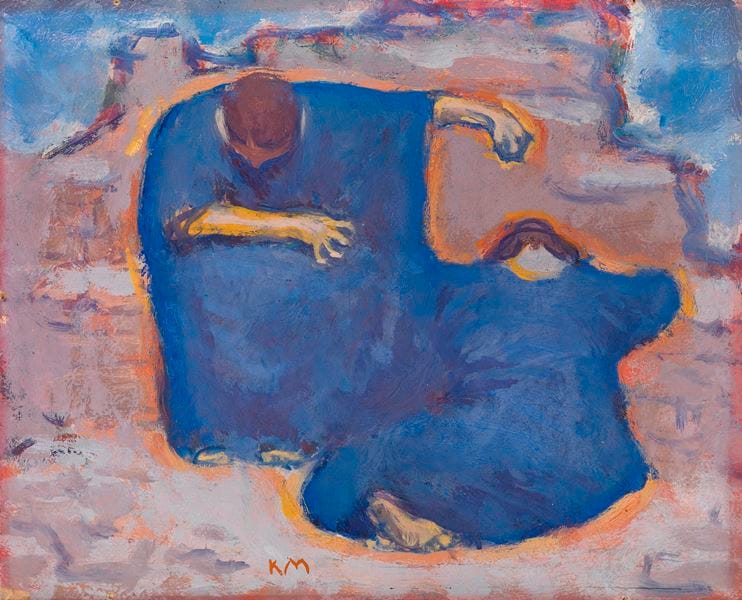
Image attribution: Koloman Moser, Trauernde Frauen, c. 1913 [Public domain], via Wikimedia Commons



