
On brain transformation during perimenopause
When I unsuspectingly found myself in perimenopause, I thought I had lost my mind! I lost all my energy, suffered from brain fog, grew forgetful, was emotionally all over the place, and experienced intense migraine attacks every few weeks. I no longer recognised myself at all. This intense experience drove me to delve deeper into the effects of the perimenopausal transition on the brain. As a neurobiopsychologist, I immersed myself in the books of neuroscientist and nutritionist Professor Lisa Mosconi, who, along with her team in the US, is pioneering neuroscience research in women. She challenges “bikini medicine,” which overlooks fundamental differences in how women’s bodies function by focusing only on the areas covered by a bikini. Neuroscience research on the female brain is still in its infancy, because medicine has long been primarily male-focused, and techniques for studying the female brain are still rapidly evolving.
Professor Lisa Mosconi is pioneering neuroscience research in women and by doing so she challenges “bikini medicine,” which overlooks fundamental differences in how women’s bodies function by focusing only on the areas covered by a bikini.
This blog is based on Mosconi’s books and international clinical insights. Writing this has helped me come to terms with the changes in my body. My hope is to foster greater understanding and compassion for women during perimenopause.
On Brain Transformation During the periMenopause
From around the age of 35, women’s levels of sex hormones—specifically oestrogen and progesterone—begin to decline (Mosconi, 2024 – The Menopause Brain). This is because the supply of eggs in the ovaries, which are largely responsible for oestrogen levels in the female body, starts to diminish. It is well known that a woman’s fertility decreases during this period, typically until around the age of 52; this phase is also referred to as perimenopause. Most women have fully reached menopause between the ages of 40 and 58 and are infertile from that point onward. The perimenopausal phase lasts, on average, between 2 and 10 years and varies widely among women, although mothers and daughters within the same family often experience a similar pattern. It is therefore a misconception that women only begin to experience menopausal symptoms in their fifties. I personally noticed changes before I turned 40—and no, I was not too young for that!
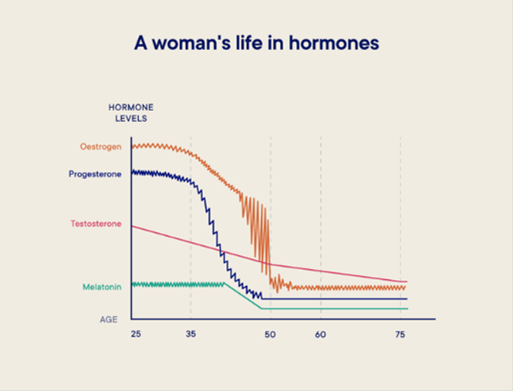
From the average age of 35, female sex hormone levels begin to decline, with significant hormonal fluctuations occurring during perimenopause. The source of this figure is unknown, but its content closely aligns with what Prof. Mosconi describes in “The Menopause Brain”.
During perimenopause, hormone levels fluctuate dramatically—just take a look at the graph above, which illustrates a woman’s life in hormones. These fluctuations occur because the feedback loop between various female hormones has gone topsy-turvy as a consequence of the lowered oestrogen levels. The pituitary gland in the brain responds by producing excessive amounts of hormones (FSH and LH) to stimulate the ovaries to mature the remaining eggs. If successful, this results in a surge of oestrogen and progesterone. But if it fails—and this happens increasingly often towards the end of perimenopause—oestrogen and progesterone levels plummet to new lows. During perimenopause, it seems the female body is doing everything it can to maintain hormonal balance and perhaps achieve one last (final) pregnancy.
During perimenopause, a women’s brain must, in a sense, ‘rehab’ from sex hormones and a true brain transformation takes place.
During perimenopause, the female brain prepares for a life with very low levels of female sex hormones in the body: a true brain transformation takes place (Mosconi, 2024). The female brain, after all, runs on oestrogen. The brain’s energy supply and blood flow depend on the presence of the female sex hormone oestrogen—specifically, the type known as estradiol. Estradiol acts as a helper, facilitating the uptake of glucose into cells, and glucose is the brain’s primary fuel. Additionally, female sex hormones keep the heart and blood vessels in our bodies supple. This is, of course, crucial for the brain, which relies on a fine network of small blood vessels and capillaries for its blood supply—and thus for the availability of oxygen and nutrients. Additionally, estradiol plays a key role in neuroprotection (by influencing the immune system and preventing oxidative stress), cell growth, neuroplasticity, communication between cells (by affecting neurotransmitters), and mood (by influencing serotonin). A sudden drop in estradiol levels in the female brain therefore has a major impact on how women feel—they must, in a sense, ‘rehab’ from sex hormones.
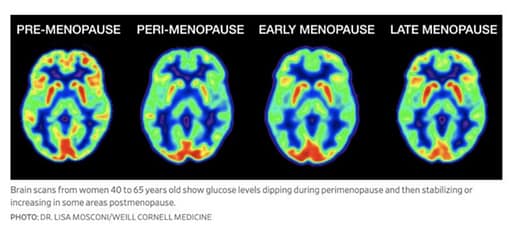
This figure was posted on social media by Prof. Dr. Mosconi’s research group and is based on the PloS One publication in 2017, see references.
Research into the nature of brain transformation during perimenopause is still in its infancy. Nevertheless, early, small-scale neuroscientific studies show that a sharp decline in estradiol levels has a major impact on the female brain. PET research involving a small group of women (N = 43) revealed that brain energy dramatically decreases during perimenopause (Mosconi et al., 2017; see the figure above). However, these changes appear to be temporary: in 80% of the women studied, brain energy levels returned to their previous state. In another ground breaking study, Mosconi and her team used a new technique—the F-FES PET scan—to visualise estradiol receptors in the brain for the first time. They found a marked increase in estradiol receptors in postmenopausal women (n = 18) compared to women before or during perimenopause (n = 36) (Mosconi et al., 2024; see the figure below). The sample sizes in these studies are small, as PET scans are expensive, invasive, and burdensome for participants. More research of this kind is needed to gain a clearer understanding of the female brain transformation and to bring an end to the era of “bikini medicine.”
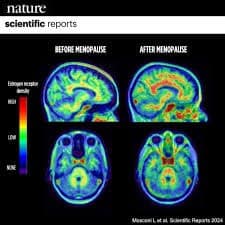
F-FES PET scans of pre- and postmenopausal women’s brains, illustrating the density of estradiol receptors before and after the menopause. This figure was shared on social media by Prof. Mosconi’s research group and is based on the Nature publication from 2024, see references.
Brain Symptoms During the Menopause – The Latest Figures
While it is widely known that perimenopause often comes with physical complaints—such as irregular menstrual cycles, hot flushes, and night sweats—far less attention is given to the common mental symptoms that are a direct result of the brain transformation described earlier. For some women, this process is relatively smooth, but for others, energy levels during perimenopause fluctuate wildly, from extreme lows to highs—resulting in, as I experienced, a mental rollercoaster! The symptoms associated with these hormonal fluctuations are quite something: the most recent clinical checklist (Newson, 2025) lists a staggering 84 symptoms. This checklist can be found on the website of Dr. Louise Newson, a women’s health specialist who investigated these symptoms in her UK clinic among more than 1,000 perimenopausal and menopausal women. Here are some of the key figures:
- The most common symptom among women seeking help during the menopause is fatigue or low energy (95%);
- Next in row are brain fog symptoms, including memory problems (94%), difficulties concentrating (92%), and word-finding difficulties (90%);
- Following brain fog are mood-related problems, such as irritability (93%), anxiety (92%), mood swings (90%), low motivation (89%), and feeling tense/nervous (88%);
- Surprisingly, the most well-known menopause symptoms—hot flushes and night sweats—appear much further down the list, though they still affect more than half of the women seeking help: night sweats (62%) and hot flushes (55%).
Hot flushes are actually a brain symptom, since they are caused by dysregulation of temperature control in the hypothalamus—a brain structure (Professor Lisa Mosconi, 2024 – The Menopause brain).
These figures are based on women seeking support from a clinic in the UK, but population-based studies among US women also demonstrate that these complaints are widespread. A remarkable 60% of women experience brain fog, 50% suffer from sleep problems and fatigue, and 20% experience mood issues or anxiety (Mosconi, 2024). By the way, 85% of perimenopausal women in population-based studies (which is quite some more than reported in the women’s clinic) experience hot flushes, which are actually a brain symptom, since they are caused by dysregulation of temperature control in the hypothalamus—a brain structure. Women aged 35 and older struggling with hot flushes, fatigue, brain fog, and mood problems are therefore not losing their minds. In fact, according to the figures, it is entirely normal.
Perimenopause as a natural life stage: the queenager brain
In many ways, the perimenopause is like puberty—a natural life stage marked by brain transformation. It is both a time of vulnerability and a time of new opportunities. Just as teenagers are not ill and do not need to be “fixed” or “repaired,” neither are perimenopausal women. For this reason, in the UK, women in this stage are sometimes called “queenagers” (NOON, 2025). Both teenagers and queenagers need space to (re)discover themselves. The mental symptoms a perimenopausal woman experiences can be viewed as signals from the brain that her lifestyle needs to change (Mosconi, 2024). If she continues to push herself with low brain energy as she did before perimenopause, she will burn through all her reserves, making her more vulnerable to burnout, depression, or even psychosis. Rather than assuming she is losing her mind, we need to remind these women that this is the queenager brain inviting her to adapt her lifestyle and rediscover herself—she will emerge wiser!
References
The books by Professor Lisa Mosconi are marked with * are highly recommended for further reading. References marked with ** are based on women’s personal or clinical experiences during perimenopause.
*Mosconi, L. (2020). The XX brain. The groundbreaking science empowering women to prevent dementia. CPI Group (UK)
*Mosconi, L. (2024). The menopause brain. The new science empowering women to navigate midlife with knowledge and confidence. CPI Group (UK)
Mosconi, L., Berti, V., Quinn, C., McHugh, P., Petrongolo, G., Pupi, A., Osorio, R., Isaacson, R.S., Vallabhajosula, S., de Leon, M.J., Brinton, R.D. (2017). Altered Brain bioenergetics in the Perimenopauze to Menopauze transition: Implications for the increased Alzheimer’s risk in women. PLoS ONE 12(10): e0185926. https://doi.org/10.1371/journal.pone.0185926
Mosconi, L., Nerattini, M., Matthews, D.C. et al. (2024). In vivo brain estrogen receptor density by neuroendocrine aging and relationships with cognition and symptomatology. Sci Rep 14, 12680. https://doi.org/10.1038/s41598-024-62820-7
**Newson, L. (2025, retrieved on 29 augustus 2025). Revealed: frequency and severity of menopauze symptoms. https://www.drlouisenewson.co.uk/knowledge/revealed-frequency-and-severity-of-menopause-symptoms
**NOON (2025, retrieved on 2025). What is a Queenager. https://noon.org.uk/what-is-a-queenager/
The featured image of this blog has been reproduced with the permission of Dr. Louise Newson. Source: https://www.drlouisenewson.co.uk/knowledge/revealed-frequency-and-severity-of-menopause-symptoms



